Abstract

INTRODUCTION: The use of pediatric inspired regimens in adolescent young adults and adults has improved outcomes in acute lymphoblastic leukemia (ALL). CALGB 10403 was prospectively tested in patients 17-39 years, showing a 3-year event free survival of 59%.
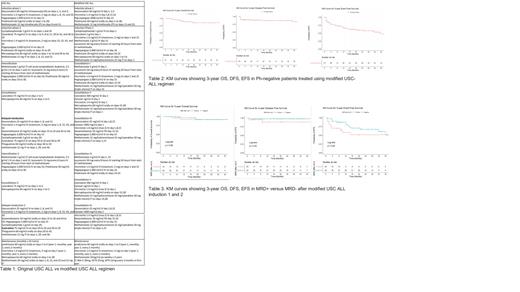
In 2007, our institution reported outcomes after incorporating peg-asparaginase (PEG) dosed at 2000mg/m 2 in induction for patients aged 17- 55 years. This regimen was well tolerated and resulted in a complete remission (CR) rate of 96%. In 2014, we reported experience with the use of multiple doses of PEG (CCG-1882) for newly diagnosed ALL adult patients, with a 7-year overall survival (OS) of 51%. Since our last report, the USC ALL regimen consisting of 2 induction phases, has been further modified with a goal of maintaining good outcomes, and improving compliance and toxicities. Fractionated doses of cytarabine were changed to a single dose, the methotrexate dose of 1g/m 2 (2.5 g/m 2 if T-cell) given D1,15 of intensification phases was changed to 3g/m 2 (B and T cell) given in single doses, and consolidation was increased to six cycles allowing for PEG holidays (Table 1).
Moreover, the approval and incorporation of novel agents such as blinatumomab and inotuzumab also changed outcomes in ALL. Therefore, this study reports an update of outcomes since further modification of the USC ALL pediatric-based regimen in the era of novel agents.
METHODS:
This is a retrospective review which included adults aged >18 with newly diagnosed Philadelphia negative ALL between 2016 and 2020 treated at USC/Norris Cancer Center and Los Angeles County Hospital (LAC). Primary objectives were over-all survival (OS), event-free survival (EFS), disease-free survival (DFS) at 3 years, and secondary outcomes were complete remission/complete remission with incomplete recovery (CR/CRi) rates and minimal residual disease (MRD) by flow cytometry. OS, DFS, EFS were reported through Kaplan Meier curves and Log-rank tests. Two-sided p value ≤0.05 was significant.
RESULTS: 121 patients with Ph-negative ALL were identified (49.6% Ph-negative B-ALL, 24% Ph-like B-ALL, 0.8% B cell lymphoblastic leukemia (LBL), 9.1% T cell ALL, 4.1% T cell LBL, 4.1% early T-cell, 5.8% mixed phenotype acute leukemia (MPAL). Median age at diagnosis was 38.5 years and maximum age of patient to receive pegasparagase during induction 1 was 63 years. 71.9% Hispanic, 15.7% white, 9.9% Asian, 2.5% African American. 57.9% males, 42.1% females. 3.4% were favorable, 4.2% intermediate, 54.6% unfavorable and 37.8% unknown by karyotypic risk stratification. Median BMI was 28.9 kg/m 2.54.6% had hepatic steatosis either on history or imaging and 5.1% had CNS disease pre-induction.
Post-induction 1, 81.4% of patients achieved CR/CRi and 50% MRD negative. Post induction 2, 82.2% achieved CR/CRi, 67.7% MRD flow negative. Post-consolidation 1, 90.9% were MRD flow negative. 33.1% subsequently received blinatumomab for MRD positive disease, 5% given inotuzumab for relapsed disease, 32.2% underwent allogenic hematopoietic stem cell transplant (allo-HSCT). Median number of pegasparagase doses received during treatment was 2, rate of relapse and mortality was 27.3% and 13% respectively.
Median OS and DFS were not reached but median EFS was 35 months. 3-year OS was 85.3%, when stratified according to MRD post induction 2; 3-year OS was 91.7% for MRD positive patients and 91.2% for MRD negative patients (p=0.55). 3-year DFS was 83.2%; 88.2% for MRD positive patients and 97.4% for MRD negative patients (p=0.22). 3-year EFS was 47.3%; 51.3% for MRD positive patients and 50.6% for MRD negative patients (p=0.49) (Tables 2-3).
Use of pegasparagase resulted in grade 3/4 toxicities including hypersensitivity (4.1%), transaminitis (21.5%), pancreatitis (5.4%), hypertriglyceridemia (49.5%), hypofibrinogenemia (45.5%), hyperbilirubinemia (21.5%) and thrombosis (16.5%).
CONCLUSIONS:
Pediatric-based modified USC ALL induction regimen led to a high 3-year OS (85.3%), DFS (83.2%) and EFS (47.3%) with predictable toxicity and compares favorably with original USC ALL regimen, CALGB 10407, GRAALL 2005 and USC/MSKCC regimen.
Interestingly, MRD positivity after induction 2 did not adversely affect OS, DFS or EFS, which is likely due to incorporation of blinatumomab and inotuzumab. These agents could have allowed for deeper remissions allowing Ph-negative patients with residual disease to receive allo-HSCT.
Chaudhary: Oncotartis: Consultancy; Pancella: Consultancy; Moderna: Current equity holder in publicly-traded company; Celldex: Current equity holder in publicly-traded company; TCR2: Current equity holder in publicly-traded company; Allogene: Current equity holder in publicly-traded company; Athelas: Consultancy, Current holder of stock options in a privately-held company; Angeles Therapeutics: Current holder of individual stocks in a privately-held company, Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees, Other: Founder, Patents & Royalties: Cell therapy . Douer: Servier: Consultancy, Speakers Bureau; Amgen: Consultancy, Speakers Bureau; Adaptive: Current holder of individual stocks in a privately-held company, Current holder of stock options in a privately-held company, Speakers Bureau; Jazz: Consultancy. Yaghmour: Novartis: Consultancy, Speakers Bureau; BMS: Speakers Bureau; Alexion: Speakers Bureau; Astellas: Speakers Bureau; Takeda: Consultancy, Speakers Bureau; Jazz: Speakers Bureau; Agios: Consultancy, Speakers Bureau.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract